Understanding Cognitive-Behavioural Therapy in Addiction Recovery
Cognitive-behavioural therapy (CBT) is a cornerstone of evidence-based addiction treatment, offering individuals a structured and goal-oriented approach to overcome substance use disorders. At One Step Rehab, we believe that targeting the cognitive processes underlying addiction can greatly enhance recovery outcomes. CBT helps clients talk openly about their issues, allowing for the identification and transformation of the negative thought patterns that drive harmful behaviours.
By developing strategies for change, individuals in therapy learn skills for coping, reducing cravings, and preventing relapse. Whether facing opioid addiction, alcohol dependence, or unresolved emotional issues, CBT tends to empower clients with the tools needed for long-term recovery, making it a vital component in modern rehab programs.
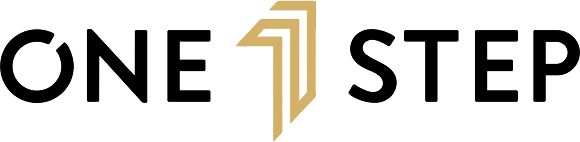
How CBT Works to Transform Negative Thinking Patterns
CBT works by systematically identifying and challenging the negative thought patterns that often underlie addictive behaviours. In my clinical experience at One Step Rehab, I’ve seen how Cognitive Behavioral Therapy targets those automatic beliefs and assumptions that can perpetuate self-destructive cycles. For example, individuals may internalise ideas like “I can’t cope without using” or “I’ll always fail at recovery.” Such thoughts can fuel cravings and create emotional distress, making it harder to stay sober.
CBT targets negative thought patterns that drive harmful behaviors by teaching clients to notice these internal messages and critically evaluate their validity. This process helps clients separate facts from unhelpful cognitive distortions and replace them with more adaptive, affirming beliefs.
During therapy treatment, clients and therapists work collaboratively to “map out” the specific thought patterns linked to substance use triggers. For example, after a stressful day, a client might think, “Drinking is the only way to relax.” CBT helps clients talk about these patterns and then develop healthier alternatives like, “I can manage stress through relaxation techniques or supportive conversations.”
Over time, this ongoing dialogue creates new mental habits, making old patterns less automatic and more preventable. Repeated exposure to these cognitive exercises builds robust coping skills.
Programs using CBT integrate homework assignments and behavioural experiments, encouraging clients to practise skills in real-life situations. This not only reinforces the therapy’s lessons but also helps clients gain confidence in their ability to resist urges and remain resilient after detox.
In dealing with powerful cravings, whether it can help alcoholics cope or resist other drug substances, these learned skills become vital in everyday recovery. Importantly, CBT tends to be highly individualised. Therapy CBT is tailored to each person’s unique history, unresolved emotional issues, and current challenges. Some clients need to address deeply rooted anxieties or depression that fuel their addiction, while others benefit from focusing on practical relapse prevention.
By making these interventions relevant and personal, the pograms CBT ensures is that every individual would end up feeling empowered and supported throughout their rehab experience. Our CBT programmes at One Step Rehab emphasise ongoing skill development. Sessions often include role-playing high-risk situations, identifying social or environmental triggers, and building plans to navigate setbacks.
This focus on concrete skills helps clients reconstruct their environment and mindset, lessening the influence of negative thinking altogether. Even after formal sessions end, continued practice ensures the lessons learned through CBT remain accessible throughout the journey of recovery.
Ultimately, Cognitive-Behavioural Therapy is more than just managing thoughts; it’s about building a foundation for a fulfilling, substance-free life. Through this process, individuals not only overcome addiction but also strengthen their overall emotional resilience, self-efficacy, and sense of purpose, key ingredients in lasting recovery. As a therapist, I’ve witnessed the transformative impact CBT work has, offering hope to individuals determined to reclaim their lives and break free from the cycle of addiction.
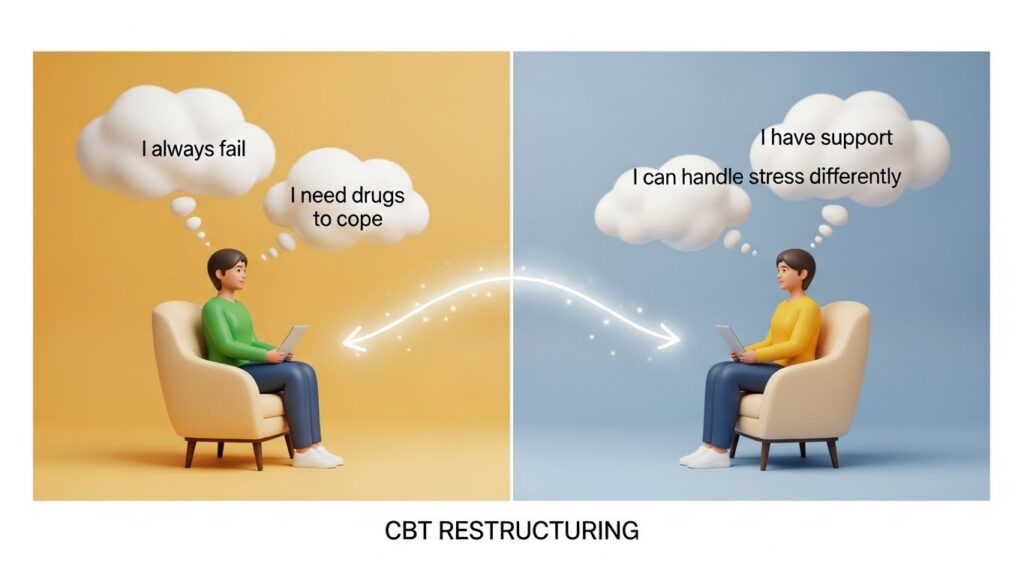
Exploring DBT: Principles and Unique Approaches
Dialectical Behaviour Therapy (DBT) stands apart from other evidence-based approaches with its unique blend of acceptance and change strategies tailored for individuals struggling with addiction. At One Step Rehab, we incorporate DBT to address not only substance use but also the complex emotional and interpersonal challenges that fuel addictive behaviours.
DBT’s foundations rest on principles such as mindfulness, emotion regulation, and distress tolerance, all of which support sustainable recovery. By combining these powerful principles, DBT empowers individuals to navigate the stressors and urges tied to addiction, laying the groundwork for lifelong wellness and transformation during detox, recovery, and beyond.
The Role of Mindfulness and Emotion Regulation in DBT for Addiction
Mindfulness and emotion regulation are central to Dialectical Behaviour Therapy (DBT), offering a robust therapeutic framework for individuals working through addiction at One Step Rehab. Unlike approaches that simply oppose substance use, DBT equips clients with core skills that foster long-lasting change and emotional stability, crucial for overcoming addiction and building a resilient foundation for recovery.
DBT’s roots in dialectical behaviour theory emphasise balance between acceptance and change, encouraging individuals to fully experience present moments without judgment and to regulate overwhelming emotional responses that often trigger substance use.
A fundamental aspect of DBT is mindfulness. By integrating mindfulness skills, individuals learn to observe their thoughts, urges, and emotions in real time without immediately reacting or turning to addictive behaviours.
In therapy dialectical sessions, we encourage clients to notice cravings, sadness, or anger as they arise and to sit with these emotions instead of succumbing to impulsivity. Mindfulness gradually increases self-awareness and control, empowering clients to make more intentional choices aligned with their long-term recovery goals. Frequently, those in active addiction struggle with compulsive behaviour patterns and fractured relationships, but mindfulness in Dialectical Behaviour Therapy provides the stability needed for clearer thinking and healthier interactions.
Emotion regulation, another cornerstone of DBT, addresses the emotional volatility and distress that often accompany addiction. Many individuals find themselves trapped in cycles of intense shame, guilt, or frustration tied to relapse or substance use, making emotion regulation skills essential for recovery.
In therapy dialectical sessions, we teach individuals practical tools to identify, understand, and modulate their emotional states. Rather than attempting to suppress or avoid difficult feelings, DBT guides clients to accept and manage these emotions in healthier ways. This active approach helps reduce the likelihood of impulsive, addiction-driven responses and fosters emotional resilience, a critical asset when navigating the inevitable ups and downs of detox and early recovery.
The combination of mindfulness and emotion regulation in DBT provides a unique, proactive strategy in the context of addiction therapy. Individuals are taught how to ground themselves during distress using mindfulness and how to use emotion regulation techniques when feeling overwhelmed, stressed, or tempted. This empowers individuals to pause before acting, to evaluate situations objectively, and to use actionable skills instead of defaulting to previous addiction-driven habits.
At One Step Rehab, it’s been inspiring to witness how integrating Dialectical Behaviour Therapy enhances clients’ capacities to face cravings, tolerate emotional discomfort, and build a lasting life free from addiction. Integrating DBT skills isn’t just about moment-to-moment crisis management. These skills evolve into daily practises, supporting emotional health far beyond the clinical environment and greatly reducing the risk of relapse.
Clients become more adept at managing triggers, repairing relationships, and responding thoughtfully under stress. Recovery is not linear, and setbacks are common, but DBT’s focus on mindfulness and emotion regulation equips individuals with evidence-based tools that stay with them throughout their lifelong journey. The powerful synergy between dialectical behaviour and practical skills ensures that individuals feel supported and encouraged every step of the way, embodying the One Step Rehab commitment to comprehensive, transformative addiction recovery.
The Main Differences Between CBT and DBT for Behavioural Therapy
When comparing behavioural therapy approaches in addiction treatment program, Cognitive-Behavioral Therapy (CBT) and Dialectical Behaviour Therapy (DBT) each bring unique strengths to supporting recovery. Both methods are widely used in rehab settings at One Step Rehab, but they differ in their therapeutic frameworks, session structure, and targeted skills.
Understanding these differences is crucial for individuals and clinicians in choosing an effective route for addiction therapy. Exploring how CBT targets negative thinking patterns that drive harmful behaviors, while DBT emphasises mindfulness and emotional regulation, helps clarify the distinct benefits and ideal contexts for each approach in long-term recovery.
Key Factors Influencing the Choice Between Therapy CBT and DBT in Addiction Therapy
As a licensed therapist specialising in addiction treatment at One Step Rehab, I frequently guide individuals and their families in selecting the most suitable behavioral therapy for their needs. The choice between Cognitive-Behavioral Therapy (CBT) and Dialectical Behaviour Therapy (DBT) hinges on several key factors tied to personal history, treatment goals, and the specific challenges faced during recovery.
Both CBT and DBT fall under the umbrella of behavioral therapy, but their mechanisms target different core issues that arise during the addiction therapy process. CBT targets negative thought patterns that drive harmful behaviours by structuring sessions around the identification and restructuring of cognitive distortions. This focused approach makes CBT exceptionally useful for individuals who experience intrusive negative thoughts, self-sabotage, or habitual patterns that reinforce substance use.
When a client is ready to engage actively and CBT helps clients talk openly about their struggles, Cognitive-Behavioural Therapy guides them toward practical solutions and rapid skill acquisition. CBT tends to be shorter in duration compared to DBT; CBT works best for those seeking a more immediate, goal-driven intervention in addiction treatment. However, DBT typically takes more time than CBT, reflecting its comprehensive focus on emotion regulation, mindfulness, and distress tolerance.
Dialectical Behaviour Therapy is often chosen when clients grapple with intense emotional swings or chronic self-harm or have a dual diagnosis, such as borderline personality disorder alongside substance addiction. Individuals who find themselves overwhelmed by emotional triggers and impulsive actions may benefit more from a dialectical behavior framework, which offers structured skills for managing acute distress and preventing relapse. DBT’s dialectical approach promotes balance between acceptance of current feelings and motivation for behavioural change, making it valuable for clients with significant emotional dysregulation.
Another deciding factor between CBT and DBT therapy is the client’s learning style and life circumstances. The programs CBT follows integrates “homework” and real-life behavioural experiments, appealing to those who prefer clear, actionable assignments. Conversely, DBT’s session structure involves group skills training and individual therapy, fostering ongoing skill-building and peer support, ideal for those who benefit from shared learning experiences.
At One Step Rehab, we find that individuals with histories of trauma, failed past treatments, or high-risk relapse situations may require a blended approach, leveraging the strengths of both CBT and DBT. It’s also worth noting that CBT tends to spotlight specific thoughts or triggers underlying addictive behaviours, whereas dialectical behavior strategies aim to enhance general emotional and interpersonal awareness.
This distinction influences not only the therapy’s duration, since DBT typically takes more time than CBT, but also its overall impact on long-term recovery. While both are evidence-based pillars of modern addiction therapy, the decision ultimately rests on an individual’s symptom profile, level of motivation, and readiness to engage with either or both therapeutic frameworks.
At One Step Rehab, we tailor addiction treatment to respect these nuances, ensuring that each client’s journey is personalised and empowered. By weighing the benefits and limitations of CBT and DBT, individuals and clinicians can collaboratively design a therapy plan that supports lasting change, whether through CBT’s cognitive restructuring or DBT’s emotional regulation. This informed choice strengthens engagement, reduces dropout rates, and maximises the effectiveness of rehab and behavioural therapy overall, providing a robust foundation for lifelong recovery.
Practical Strategies for Integrating DBT and CBT in Long-Term Recovery

At One Step Rehab, we recognise the immense value in blending Cognitive-Behavioral Therapy (CBT) and Dialectical Behaviour Therapy (DBT) as a cohesive framework for addiction treatment. While previous content has explored how CBT targets negative thought patterns that drive harmful behaviours and highlighted the role of mindfulness and emotion regulation in dialectical behaviour interventions, the true potential for lasting recovery emerges when both modalities complement one another in daily life. Practical integration begins with developing strategies that capitalise on each approach’s unique strengths, ensuring every individual’s recovery is robust and sustainable over time.
One effective method of integration involves structuring therapy to alternate between focused CBT interventions and DBT skill-building exercises. For instance, CBT works efficiently to challenge entrenched thoughts like “I’ll never be able to overcome addiction,” while DBT introduces skills for tolerating distress and managing overwhelming emotions when relapse temptation strikes. This approach teaches individuals to not only reframe cognitive distortions through CBT but also to accept and regulate the feelings associated with those thoughts using dialectical behaviour principles.
During addiction treatment, therapists may use CBT to identify high-risk thought patterns and then apply DBT’s mindfulness and emotion regulation skills in real-time, building resilience against cravings and stress.
CBT and DBT often intersect when building relapse prevention plans. While CBT helps clients talk about the situations that trigger substance use, dialectical behaviour strategies equip them with actionable skills to cope, including distress tolerance, mindful breathing, and interpersonal effectiveness.
Regular therapy sessions at One Step Rehab focus on practising these integrated skills in both individual and group formats, allowing for peer support, skill mastery, and the reinforcement of healthy behaviour patterns. Over time, repeated use of CBT and DBT skills solidifies new neural pathways, empowering clients to manage cravings, avoid impulsive decisions, and remain focused on long-term goals.

Developing strategies for integration isn’t limited to formal therapy settings. Clients are encouraged to use skill cue cards, daily mindfulness check-ins, and written CBT thought records as part of their routine. In moments of vulnerability, referencing a CBT worksheet or pausing to engage a dialectical behavior mindfulness skill transforms fleeting urges into opportunities for growth. The combined approach recognises that relapse triggers arise in countless forms, thoughts, emotions, and social pressures, and that a blend of CBT and DBT provides a full toolkit for both prevention and recovery during and after addiction treatment.
Ultimately, what sets this approach apart at One Step Rehab is our unwavering commitment to comprehensive, evidence-based care. Every individual learns not just to survive addiction but to thrive by continually mastering the skills and strategies fundamental to both CBT and dialectical behavior therapy.
By integrating these powerful behavioural therapy models, clients become adept at recognising, tolerating, and transforming the core challenges of addiction, making a healthy, substance-free life their new reality.
Fact-checked by:
Dr. Worapakthorn Kongpesalaphun (M.D.) Consultant Psychiatrist.

Naranchaya Sriburapar, Ph.D.
Dr. Naranchaya Sriburapar is a Thai Licensed Senior Clinical Psychologist with over 20 years of experience in mental health and addiction treatment. She holds a Ph.D. in Cognitive Psychology/Neuropsychology from the University of Kent, UK. Her exp...
Learn more about Naranchaya Sriburapar, Ph.D.